Pulmonary hypertension is a type of high blood pressure that affects the arteries in the lungs and the right side of your heart.
Pulmonary hypertension begins when tiny arteries in your lungs, called pulmonary arteries, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through your lungs, and raises pressure within your lungs’ arteries. As the pressure builds, your heart’s lower right chamber (right ventricle) must work harder to pump blood through your lungs, eventually causing your heart muscle to weaken and eventually fail.
Pulmonary hypertension is a serious illness that becomes progressively worse and is sometimes fatal. Although pulmonary hypertension isn’t curable, treatments are available that can help lessen symptoms and improve your quality of life.
Symptoms:
The signs and symptoms of pulmonary hypertension in its early stages may not be noticeable for months or even years. As the disease progresses, symptoms become worse.
Pulmonary hypertension symptoms include:
- Shortness of breath (dyspnea), initially while exercising and eventually while at rest
- Fatigue
- Dizziness or fainting spells (syncope)
- Chest pressure or pain
- Swelling (edema) in your ankles, legs and eventually in your abdomen (ascites)
- Bluish color to your lips and skin (cyanosis)
- Racing pulse or heart palpitations
Causes:
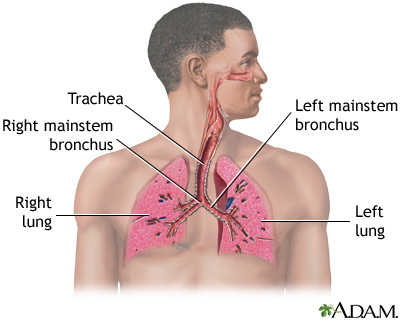
Your heart has two upper and two lower chambers. Each time blood passes through your heart, the lower right chamber (right ventricle) pumps blood to your lungs through a large blood vessel (pulmonary artery). In your lungs, the blood releases carbon dioxide and picks up oxygen. The oxygen-rich blood then flows through blood vessels in your lungs (pulmonary arteries, capillaries and veins) to the left side of your heart.
Ordinarily, the blood flows easily through the vessels in your lungs, so blood pressure is usually much lower in your lungs. With pulmonary hypertension, the rise in blood pressure is caused by changes in the cells that line your pulmonary arteries. These changes cause extra tissue to form, eventually narrowing or completely blocking the blood vessels, making the arteries stiff and narrow. This makes it harder for blood to flow, raising the blood pressure in the pulmonary arteries.
Idiopathic pulmonary hypertension
When an underlying cause for high blood pressure in the lungs can’t be found, the condition is called idiopathic pulmonary hypertension (IPH).
Some people with IPH may have a gene that’s a risk factor for developing pulmonary hypertension. But in most people with idiopathic pulmonary hypertension, there is no recognized cause of their pulmonary hypertension.
Secondary pulmonary hypertension
Pulmonary hypertension that’s caused by another medical problem is called secondary pulmonary hypertension. This type of pulmonary hypertension is more common than is idiopathic pulmonary hypertension. Causes of secondary pulmonary hypertension include:
- Blood clots in the lungs (pulmonary emboli)
- Chronic obstructive pulmonary diseases, such as emphysema
- Connective tissue disorders, such as scleroderma or lupus
- Sleep apnea and other sleep disorders
- Heart abnormalities you’re born with (congenital heart defects)
- Sickle cell anemia
- Chronic liver disease (cirrhosis)
- AIDS
- Lung diseases such as pulmonary fibrosis, a condition that causes scarring in the tissue between the lungs’ air sacs (interstitium)
- Left-sided heart failure
- Living at altitudes higher than 8,000 feet (2,438 meters)
- Climbing or hiking to altitudes higher than 8,000 feet (2,438 meters) without acclimating first
- Use of certain stimulant drugs, such as cocaine
Eisenmenger syndrome and pulmonary hypertension
Eisenmenger syndrome, a type of congenital heart defect, causes pulmonary hypertension. It is most commonly caused by a large hole in your heart between the two lower heart chambers (ventricles), called a ventricular septal defect (VSD). This hole in your heart causes blood to circulate abnormally in your heart. Oxygen-carrying blood (red blood) mixes with oxygen-poor blood (blue blood). The blood then returns to your lungs instead of going to the rest of your body, increasing the pressure in the pulmonary arteries and causing pulmonary hypertension.

Treatments:
Medications:
- Blood vessel dilators (vasodilators). Vasodilators open narrowed blood vessels. One of the most commonly prescribed vasodilators for pulmonary hypertension is epoprostenol (Flolan). The drawback to epoprostenol is that its effects last only a few minutes. This drug is continuously injected through an intravenous (IV) catheter via a small pump that you wear in a pack on your belt or shoulder. This means that you’ll learn to prepare your own medication mixture, operate the pump and care for the IV catheter. You’ll need comprehensive follow-up care. Potential side effects of epoprostenol include jaw pain, nausea, diarrhea, leg cramps, as well as pain and infection at the IV site.Another form of the drug, iloprost (Ventavis), avoids many of these problems. Iloprost can be inhaled every three hours through a nebulizer, a machine that vaporizes your medication, making it far more convenient and less painful to use. And because it’s inhaled, it goes directly to the lungs. Side effects associated with iloprost include chest pain — often accompanied by headache and nausea — and breathlessness.
- Endothelin receptor antagonists. These medications reverse the effect of endothelin, a substance in the walls of blood vessels that causes them to narrow. One of these medications, bosentan (Tracleer), may improve your energy level and symptoms. The drug isn’t for pregnant women. If you take bosentan, you’ll need monthly liver monitoring, because the drug can damage your liver. Ambrisentan (Letairis) is another medication that stops the narrowing of your blood vessels. This drug can cause serious liver damage if not taken appropriately, and it shouldn’t be taken by pregnant women. Before taking the drug, tell your doctor about any liver condition you have.
- Sildenafil and tadalafil. Sildenafil (Revatio, Viagra) and tadalafil (Cialis, Adcirca) are sometimes used to treat pulmonary hypertension. These drugs work by opening the blood vessels in the lungs to allow blood to flow through more easily. Side effects include upset stomach, dizziness and vision problems.
- High-dose calcium channel blockers. These drugs help relax the muscles in the walls of your blood vessels. They include medications such as amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and nifedipine (Adalat, Procardia). Although calcium channel blockers can be effective, only a small number of people with pulmonary hypertension respond to them.
- Anticoagulants. Your doctor is likely to prescribe the anticoagulant warfarin (Coumadin, Jantoven) to help prevent the formation of blood clots within the small pulmonary arteries. Because anticoagulants prevent normal blood coagulation, they increase your risk of bleeding complications. Take warfarin exactly as prescribed, because warfarin can cause severe side effects if taken incorrectly. If you’re taking warfarin, your doctor will ask you to have periodic blood tests to check how well the drug is working. Many other drugs, herbal supplements and foods can interact with warfarin, so be sure your doctor knows all of the medications you’re taking.
- Diuretics. Commonly known as water pills, these medications help eliminate excess fluid from your body. This reduces the amount of work your heart has to do. They also may be used to limit fluid buildup in your lungs.
- Oxygen. Your doctor may suggest that you sometimes breathe pure oxygen, a treatment known as oxygen therapy, to help treat pulmonary hypertension, especially if you live at a high altitude or have sleep apnea. Some people with pulmonary hypertension eventually require constant oxygen therapy.
Surgeries
- Atrial septostomy. If medications don’t control your pulmonary hypertension, this open-heart surgery may be an option. In an atrial septostomy, a surgeon will create an opening between the left and right chambers of your heart to relieve the pressure on the right side of your heart. Atrial septostomy can have serious complications, including heart rhythm abnormalities (arrhythmias).
- Transplantation. In some cases, a lung or heart-lung transplant may be an option, especially for younger people who have idiopathic pulmonary hypertension. Major risks of any type of transplantation include rejection of the transplanted organ and serious infection, and you must take immunosuppressant drugs for life to help reduce the chance of rejection.

Post a comment